A Nice Development in HDHPs: More Reduced Cost Sharing For Targeted Conditions
By Clive Riddle, October 7, 2021
AHIP and the Smarter Health Care Coalition have released survey results that found ‘most health insurance providers and many large employers have taken advantage of new regulatory flexibility to cover more chronic disease prevention services on a pre-deductible basis.”
The survey took aim at finding out how many plans targeted changes after the 2019 change in IRS guidance for HSAs/HDHPs. The survey report noted that “until recently, HSA-eligible health plans were restricted in covering care that wasn’t considered preventive before a consumer satisfied their plan’s deductible. But in July 2019, the Internal Revenue Service (IRS) issued Notice 2019-45, guidance which expanded the list of preventive care benefits to include many items and services used to manage chronic health conditions. Now, plans and employers may offer 14 additional items and services pre-deductible, including insulin and other glucose lowering agents, glucometers, inhalers, statins, and others.”
The good news? "Most respondents modified their HSA-eligible health plans to cover more chronic disease prevention services on a pre-deductible basis: 75% covered additional services without applying a deductible in their fully insured products, and 80% in their self-insured products."
How far did respondents go in reducing or eliminating cost sharing for targeted conditions? 44% of fully-insured and 4% of self-funded plans applied changes in all contracts, 26% of fully insured plans and 38% of self-funded plans did so in most contracts, and 30% of fully insured and 58% of self-funded plans did so in some contracts.
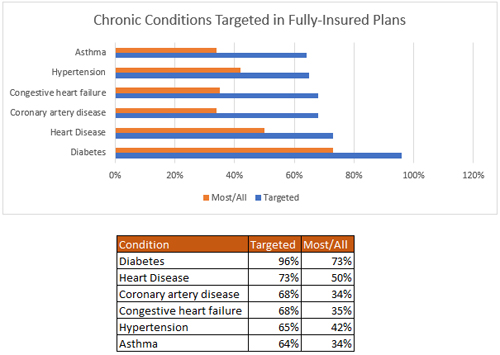
What chronic conditions were most frequently targeted? The survey report tells us that “Health insurance providers targeted a variety of chronic health conditions with two conditions targeted by almost all plans: diabetes (96% of plans in both fully insured and self-insured products), and heart disease (targeted by 73% in fully insured products and 74% in self-insured products).”
We compiled the results for fully-insured plans of the conditions targeted by more than 60% of the plans, to provided this graph of the top conditions that will have reduced cost sharing:
 Post a Comment |
Post a Comment |  Thursday, October 7, 2021 at 04:34PM
Thursday, October 7, 2021 at 04:34PM 

Reader Comments