Value-Based Care and Care Coordination: Five Key Takeaways from WakeMed Key Community Care and UC San Diego Health
By Claire Thayer, April 12, 2022
Healthcare organizations face increasing pressures to meet demands of population health and effective care management. Recently, we hosted a panel discussion webinar, co-sponsored by MCG Health, that identified some of the challenges to delivering value-based care and how providers are leveraging MCG Health solutions for care coordination to develop high-quality care programs.
We caught up with speakers Lindsey Pierce, MSN, RN, CCN, Assistant Director, Population Health UC San Diego Health and Kathryn Tarquini, PhD, RN, CCM, Director, Clinical Services, WakeMed Key Community Care on five key takeaways:
1. How did COVID-19 impact your organizations?
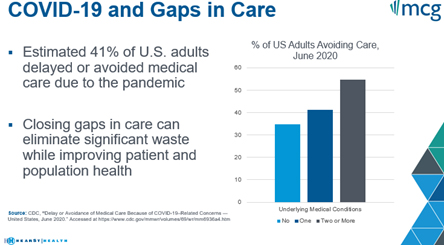
According to the CDC, an estimated 41% of US adults with one underlying medical condition avoided seeking care in 2020. This number jumps to over 50% for people with two of more underlying medical conditions. The COVID-19 pandemic is at least partly to blame for these gaps.
Lindsey Pierce: During the pandemic, we saw that patients were either delaying care or switching over to telehealth visits, and they weren't being screened as adequately. Patients were also very scared and often socially isolated, so there was a further need to use MCG psychosocial assessments to address these new gaps. Like so many organizations, we also had issues with staffing. Nursing students were unable to graduate at a time when we needed nurses, so we took a twofold approach, and we started a nursing student clinical program with our population health team who contacted patients during this time.
Amid the pandemic, we were also starting new programs and making changes to better serve our patients, and it was difficult to get everyone aligned around the needed cultural change. This is something that takes time and it's important to remember to communicate the ‘why’ behind value-based care and make sure that your team understands it. Starting out, it took a little bit of time even for providers to understand that our care managers are part of the care team and we're here to help them. Using physician champions and patient advocates helped to break down those barriers, build rapport across the teams, and now every provider wants our team involved in the patient’s care.
Kathryn Tarquini: One of the challenges we faced was launching a renewed service line - new teams, models, platforms, and tools - in early 2020, alongside the start of a pandemic. We learned to leverage our strong foundation built on the mission and vision of the ACO and the care management model. This meant we had to learn to engage virtually and build and strengthen relationships that way, using multimodal messaging to educate partners and providers about our service lines.
We also listened to what providers and practices were experiencing and needed, especially around the pandemic with things like vaccinations and other care interventions so we could provide solutions to address them when possible. Our technology platform and tools allow for transparency of our care management work, which also helped.
2. How is the transition to value-based care affecting your organization?
Lindsey Pierce: Overall the transition to value-based care has been a tremendously positive impact for UC San Diego Health (UCSD). It's allowed us to help drive some cultural changes that really benefit our patients, and it also gives us the opportunity to generate some revenue or share savings. We found that population health services have been at the forefront for helping to drive cultural change in strategy for value-based care, and we see that for interdisciplinary teams risk stratification and utilization oversight are essential to the success of the care program.
We began in 2016 as the organization started to shift towards growing our value-based contracts. We started in Medicare Shared Savings about three years ago and it helped us to expand and grow our network within San Diego, and we now have around 60% of insured lives under a value-based care arrangement. Before this shift, UCSD was performing significantly higher than the national average on hospital admissions per thousand. Over our three-year journey of aligning workflows, integrating technology, and improving processes, we’ve really been able to bring down avoidable hospital admissions to considerably below the national average.
For organizations who are starting out on this journey, it can seem like a difficult transition going from fee-for-service to value-based care. But at its core value-based care is simple, it's quality divided by cost, and this helps support high quality and cost effective care delivery. Through our population health services, we’re able to provide wrap around services to our patients and that helps us to support high quality of care. I do think we'll see this more in the future in healthcare in the coming years and it’s something that I'm excited to be a part of.
Kathryn Tarquini: WakeMed Key Community Care is an ACO formed in 2014 as a joint venture between WakeMed Health and Hospitals and the Key Physicians Group of independent physicians in the Raleigh, North Carolina area. These organizations came together because they realized the importance of delivering high quality care in a value-based care model. Since the ACO was formed eight years ago, our primary care physicians have come to understand the value of value-based care. They’re now highly experienced and have become strong advocates for this model. In 2020, we brought all population health services in-house and this resulted in the formation of new centralized teams for care management – which is when we began using MCG and Arcadia for our care management needs. This has also helped us to provide higher quality care. The overall effect on the organization is based on the results that we’ve seen in quality, achieving and exceeding quality measures, being able to provide coordinated care, and using tools to proactively care for patients. Currently, there are also a variety of population health and quality initiatives within many departments of the hospital system that are value-based, such as hospital or home and navigator programs. We're working together to align some of these initiatives and connect the leaders to more formally collaborate and create some synergy for greater success.
3. What role have your technology partners played in supporting your transition to value-based care?
Kathryn Tarquini: Our primary partners that have made our program successful are MCG and Arcadia. These two partners have been critical to creating a strong foundation, and there's a lot of synergy that comes from the alignment and integration of these two. We use MCG guidelines for clinical decision support integrated into Arcadia’s Care management platform to document, track, and manage the care management work and the care managers’ workload – this is at the core of what we do with care management.
Arcadia also provides for our data analytics and management system and allows for data exchange with each other. We have close to 20 different EMRs in our ACO and so it collects and exchanges data with the EMRs to provide proactive tools. For example, a pre-visit planning tool to proactively manage risk and a predictive analytics tool using data from claims, the EMR and census data to identify those patients who are most likely to benefit from care management. The Arcadia platform also provides a way to see the status of quality measures – specifically which quality measures are completed and which ones have a gap – so that the practices can proactively address those by reaching out to patients. It promotes care coordination with the providers and the practice partners by allowing all members of the health care team to view all aspects of the care management process in real time.
The partnership with MCG supports the team with accurate and efficient assessment tools that are easy to read and follow, written in a conversational tone, and with many evidence-based assessment options to choose from. Using MCG also allows us to have standard work at the point of care, and this is especially helpful for our team with diverse experience and expertise. We have a multidisciplinary team of RNs and LCSWs, and what we call case management representatives. Using MCG ensures that everyone is deploying the evidence-based guidelines consistently, which leads to an efficient workflow and positive work experience.
Lindsey Pierce: It’s important to have partners that understand your organization’s vision and provide tools that allow the team to be organized, efficient and perform at the top of their clinical license. In 2021, we integrated MCG care guidelines into Epic Healthy Planet, and our team was involved from the very beginning. We had super users to make sure that the product worked efficiently. We also have health coaching through text message and remote blood pressure monitoring, so we've created really nice wrap around service for our patients.
With MCG’s partnership, we refined and made sure the workflows were seamless, and it was great from a patient perspective as well. It was an absolute journey, but one of the things we always look for, whether it's the community partner and affiliated provider or vendor, it's making sure that you have a partner who's willing to work with you and reach the ultimate goal and is willing to adapt and change - in healthcare you have to be adaptable and willing to adjust as needed. We found that really great partnership with MCG. We got help and support every step of the way with our Epic super users and from our team who were working on integrating the assessments. In 2024, we're hoping to get population health accredited through NCQA, and I think that will be very well supported based upon the integration of MCG’s assessments. Our text-based health coaching platform also uses MCG’s education materials, so that's fantastic because the patients are hearing the same information consistently whether it's through the text messaging program or if we mail our educational materials. Building strategic partnerships with community organizations, network-affiliated providers, or vendors, it's really important that all are aligned to avoid duplication of services, waste, and coordinate a really seamless experience for our patients. That's something that we've certainly found through the relationships that we've developed with MCG and our other partners.
4. In what ways has predictive analytics helped your organization to improve patient outcomes?
Lindsey Pierce: It’s important to have data analytics that identifies gaps in care opportunities, performs risk stratification and identifies patients most likely to benefit from the program, and turns patient clinical data into actionable information. I think oftentimes as we enter into more value-based care contracts, each will have nuances of the data analytics they're looking for. If you can synthesize down to one overarching goal, this can help to simplify a target for your care team, and that way your team members and providers aren't feeling confused about what they're working towards. We've done that with UC San Diego Health - simplified to just a few simple goals - and we apply them to all of our value-based care agreements and our team is really clear on what we're working towards. They're easy to measure, and it gives us a good place to work on process improvement. We focus primarily on one goal that's lowering all costs: hospital admissions per thousand. We do this because it's very well-defined, easy to measure, and is a metric where our team can make a direct impact. There might be some goals that you maybe don't have great data analytics on; even though it might be a good goal, if you can't share the outcomes, that can make that goal really difficult to work towards.
Kathryn Tarquini: We use data analytics in real-time and just-in-time opportunities to optimize care and proactively manage risk to drive population health management, and predict which patients are most likely to benefit from care management services. One tool that our practices use is the ‘pre-visit planning tool,’ which helps the care team identify quality care gaps and risk coding opportunities just before an office visit. So far, this has helped us achieve exceptional quality scores and lower readmission rates across numerous payers, and we’ve been able to distribute shared savings to participating providers each year. For example, between 2016 and 2019, we distributed nearly $120 million in shared savings from BCBSNC contracts alone.
5. What are some of the major milestones, key players, and successes you’ve seen implementing enterprise-wide value-based care model?
Lindsey Pierce: Key milestones were the development of our community network (community partnerships), growing our team and getting our workflows to be standards-based, along with integration with telemedicine to extend our reach without adding FTEs. We needed involvement from every level, physician champions, leadership, great vendors that can address gaps, and care managers. We found that having solid relationships with our network is one of the first steps we needed to take, and it was really important for us to regularly meet and facilitate goal alignment with that network. That way we were able to share performance milestones and make sure that every provider within the network understood the benefits and also the potential risk. We really focus on having our care team members work to the top of their licensed scope of practice and we also want to give them the tools to have a direct impact on process improvement for our team. We sent them all to LEAN 6 Sigma training and this just helps the team to understand the tools and resources on how to create change as you work towards standardized work in a new program. We joke all the time on our team that the only thing that's consistent is change because we're continually refining our workflows to be lean and patient-centered.
Kathryn Tarquini: There are two main factors that contribute to our success. The first is our providers, and the fact that we’re a physician-led ACO. Our providers are experienced advocates for value-based care – and we have strong relationships with them and their practices. Our model places the patient/PCP relationship at the core of our work. Providers review patients who've been identified for care management by our predictive analytics, and when possible, they alert patients of our pending outreach.
Another factor contributing to our success is the compassionate and highly-skilled care management team we’ve assembled. We help them have a positive experience, professional fulfillment, and joy through this work by equipping them with MCG and other tools, educating them about strategies, skills and trends, and we problem-solve together. By creating a work environment that focuses on continuous quality improvement, fosters collaboration and innovation, and where it's safe to learn and grow from opportunities, we’re able to fulfill our mission and deliver timely, high-quality care to our patients.
We've been seeing upwards of 50-70% engagement with patients through care management, and we have numerous patient stories demonstrating how the team has been able to make a difference in our patients’ lives. We decided last year to reinvest shared savings to provide actual solutions to identify social determinants of health (SDOH)-related barriers. We've been excited to launch two initiatives this year, including a rideshare for transportation support, and a meal service for delivering medically-tailored meals to patients’ homes. We are really looking forward to seeing some of the specific examples and impact that these and other interventions are having on our patients’ health and their health outcomes.
If you missed this informative webinar, we invite you to watch this short recap video here. Additionally, below is a list of webinar supplemental material that may interest you:
MCG White Paper. Populations at Risk: Optimizing Post-Acute Care Management
On-Demand Physician Leader Webinar Series. Populations at Risk: Optimizing Post-Acute Care Management
MCG White Paper. Population Health: Engaging Patients to Improve Healthcare Outcomes
The MCG Guide to Efficient Care Coordination & Patient Throughput

 Share This Post
Share This Post 
Reader Comments