Catching up with Advisory Board’s Ken Leonczyk on the State of the Health Plan Industry and what health plan leaders need to know for 2022
By Claire Thayer, April 11, 2022
The pandemic has had a significant impact on health plans and in many ways has been a catalyst for change across the healthcare industry. Recently, Ken Leonczyk, Executive Partner, Advisory joined us for a lively discussion on what health plans need to know about key structural shifts of the peri-pandemic period. Ken identifies these six strategic points of inflection that will shift industry structure in the years ahead.
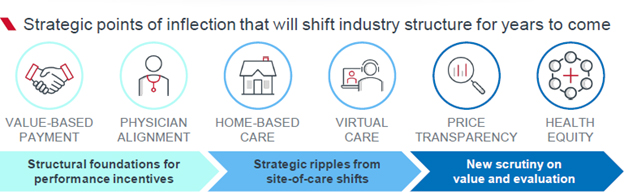
Value-Based Payment
Risk-based payment models will continue to grow, but who participates is an open question. The pandemic has done little to shift long-standing barriers in hospital financial needs, but plans have made headway with independent physician groups. Plans must now think about how the growing array of models fit together in a complex ecosystem.
Physician Alignment
An array of non-hospital suitors—plans, private equity firms, service partners, and national groups—are aligning more closely with physicians through a variety of partnership models. While hospitals may lose power, plans need to prepare to navigate relationships with all manner of new stakeholders throughout physician networks.
Home-Based Care
The wave of investment in home-based care today, centered around start-up financing or grants, does not guarantee long-term, systemic change. The industry may exacerbate existing challenges around staffing supply, care fragmentation, and health inequities. Plans must weigh how their policies will impact network access and marginalized patients.
Virtual Care
Most of the pandemic’s spike in virtual care came from traditional providers, but vendors are angling to transform their offerings to steal patient relationships— not just visits. As plans explore virtual-first products, they must ensure incentives are enough to influence consumers—and brace for fallout with local providers.
Price Transparency
The market will soon be inundated with an unprecedented level of pricing information, but disruption to historic practices will depend on the usability of the data. New vendors are emerging to parse and package the data for end users, so plans must prepare to clarify the broader context of their rates to members, purchasers, and providers.
Health Equity
The past few years brought health equity into stark focus, but to make true progress, leaders must cement equity as a business goal. As plans build equity goals into provider payments and care management actions, they must standardize data collection and analysis to generate evidence for sustainable interventions.
If you missed this informative webinar presentation, State of the Health Plan Industry: Unpacking the potential impact for 2022 planning, we invite you to watch this short webinar recap video here.
You can access the complimentary presentation slides presentation slides here and webinar video here. To continue the conversation with Ken Leonczyk and learn more about how Advisory Board is working with other health care organizations, drop him an email at healthplan@advisory.com.

 Share This Post
Share This Post 
Reader Comments