On the Journey of Cost Containment - China’s DRG Development and Implementation
By Rong Yi and Wendy Liu, September 16, 2021
Diagnosis Related Groups (DRGs) was first introduced in the US in the 1980s as a payment methodology for Medicare. After decades of development, implementation and operational improvement, it remains one of the most dominant payment mechanisms by government and private payers, and is also widely used as an analytical and measurement tools in the healthcare industry.
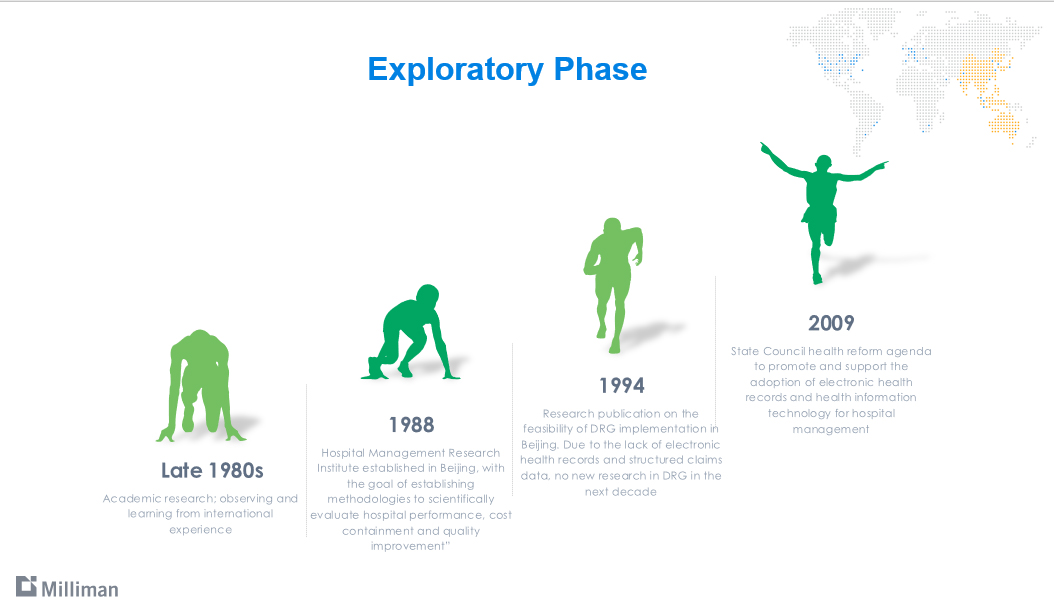
Health policy researchers in China started exploring the DRG methodology in the late 1980s. At the time, coverage and benefit levels varied significantly by employment status and place of residence. Structured claims data with standardized codes were not available back then to support deeper analysis, although the feasibility of implementing DRG was studied in the early-to-mid 1990s[1].
In 2009 China’s State Council issued a set of sweeping healthcare reform proposals[2], laying out the foundation of the new basic social health insurance scheme, which is in existence today. Included in the proposals were emphasis on equity, efficiency and quality in public hospital management, as well as investing in information technology for the healthcare sector. DRG research and development took off since then. As China went through rapid economic growth, significant urbanization and aging of the population, healthcare expenditure keeps rising steadily. There is a strong need for cost containment. Core to China’s basic social health insurance scheme is coverage for inpatient services. It is not surprising that DRG is prioritized as a payment methodology.
In the past 20 years, several independent research teams have developed and piloted their own versions of DRGs – BJ-DRGs, C-DRGs, CN-DRGs, CR-DRGs, to name a few. Hospital information system vendors, insurance companies working as third-party administrators for local social health insurance bureaus, and other technology companies invested and competed in hospital management system solutions based on these various versions of DRGs. In October 2019 the National Social Health Insurance Bureau rolled out CHS-DRG, the official version for national adoption. The diagrams below highlight a number of key milestones in the exploratory phase and the roll-out of the national standard.
CHS-DRGs’ grouping relies on the ICD-10 diagnosis codes[3] and ICD-9-CM-3 procedure codes on hospital inpatient discharge records. Similar to the DRG methodologies used in other parts of the world, CHS-DRGs also looks for secondary diagnoses, secondary procedures, complications/comorbidities, and sometimes individual factors (gender, and birthweight for neonates) to determine the severity of a hospital admission. There are 618 DRGs in the current methodology, falling into 26 Major Diagnostic Categories (MDCs). 229 are surgical DRGs.
It is worth pointing out that the implementation of the CHS-DRGs national standard allows for local flexibility to reflect differences in data quality and readiness. For instance, where data is not of reasonably good quality or has small number of cases, consolidation of existing DRGs would be permitted. Local flexibility is a practical approach to implementing a sophisticated and data-driven methodology such as the DRGs. After all, China is vast geographically. There are more than 34,000 hospitals, more than 954,000 community health facilities, and almost 16,000 specialized public health facilities, with a total of 8.8 million hospital beds at the end of 2019[4] . Different localities and facilities are at different stages of health information technology adoption. According to an industry report[5], during 2017-2018, only 39% hospitals implemented electronic medical record systems.

Looking Ahead
DRG is not only a grouping methodology and a payment mechanism, it also has significant impact on the management and operations of a healthcare system. As it relates to hospital inpatient services, the core to China’s basic social health insurance, its impact can be wide and deep.
On the data front, as more and more cities implement DRG, it is reasonable to expect that hospitals and other healthcare facilities will increase in their adoption of electronic medical records systems. An emphasis on standardized, quality and accurate coding of diagnoses and procedures has already become apparent amongst the hospitals that are running DRG pilots. We see both pros and cons of this digitization trend.
- Pros – more structured and standardized data becomes available which will help the entire healthcare ecosystem measure and compare cost, quality and value of healthcare service. For commercial health insurance, insurance brokers, drug and device manufacturers, and telehealth, structured data is particularly important to business success.
- Cons – DRG implementation requires resources and expertise, which could create further polarization of healthcare facilities in that better endowed facilities will be moving on a faster track in terms of finance and management than others
In other countries that introduced DRGs to replace an existing fee-for-service payment system, it is expected that DRG based payments can help reduce the inefficiencies associated with excessive (and sometimes unnecessary) provision of services (especially diagnostic tests) and drug prescribing, as well as long hospitalizations. It is also expected that perverse incentives may arise with the introduction of DRGs in different countries, such as providers cutting down on necessary services, or prematurely discharging patients from the hospital, or cherry-picking of patients[6].
There has been anecdotal reports on gaming of the DRG system. For instance, patients were discharged earlier than medically appropriate due to length of stay limitations introduced by the DRG pilots[7]. There are also concerns with respect to upcoding to receive higher DRG payment. Given the newness of DRG implementation, well-documented empirical evidence on gaming of the system is not available. It remains to be seen whether the implementation of DRG would result in lower care quality or whether low-value care would be “squeezed” from the inpatient setting to the outpatient setting.
If DRG implementation can lead to successful cost containment in the inpatient setting, it would benefit both the government and private payers. A very important type of commercial health insurance product in China is high deductible hospital inpatient coverage. Better cost containment could potentially lead to fewer claims reaching the deductible.
[1] Numerous articles referenced a collection of feasibility studies conducted by the Beijing Hospital Management Research Institute in 1994 titled “Articles on the Feasibility of DRGs in Hospital Management in Beijing”. The articles cannot be retrieved online. The Beijing Hospital Management Research Institute is now under the Beijing Municipal Health Commission Policy Research Center (http://www.phic.org.cn/zzjg/lsyg/), one of the main contributors of China’s DRG research over the years.
[2] http://www.gov.cn/jrzg/2009-04/06/content_1278721.htm
[3] China uses the ICD-10 WHO version with its own modifications. The latest version is called ICD-10 GB/T 14396-2016. The implementation of the modified ICD-10 WHO code set started in 2001.
[4] http://www.nhc.gov.cn/guihuaxxs/s10748/202006/ebfe31f24cc145b198dd730603ec4442.shtml
[5] “2020 China’s Electronic Medical Record Adoption and Future Trends”, chyxx.com
[6] Bredenkamp, Caryn, Sarah Bales, and Kristiina Kahur, eds. 2020. Transition to Diagnosis-Related Group (DRG) Payments for Health: Lessons from Case Studies. International Development in Focus. Washington, DC: World Bank. doi:10.1596/978-1-4648-1521-8.
[7] For instance, https://news.dayoo.com/guangzhou/202108/17/153828_54021117.htm, and https://china.huanqiu.com/article/44O20Ko4h3f

 Share This Post
Share This Post 
Reader Comments